Case Report : Photobiomodulation Therapy for Vascular Type Dementia, Improvement in Cerebral Blood Flow by SPECT Scan
- drashleighbhanjan2
- Aug 25, 2025
- 9 min read
Updated: Aug 26, 2025
Introduction
The main goal of vascular dementia treatment is managing the potential underlying causes, whether it be hypertension, diabetes or other systemic conditions. Included in the treatment regimen is providing supportive measures such as physical or occupational therapy meant to keep the patient from declining further, or for patients who also suffered a cerebrovascular accident, for rehabilitation. Although there is no evidence that nonvascular factors may contribute to cognitive decline, some clinical trials seem to support the use of medications meant for other types of dementia like Alzheimer’s may also offer a modest benefit in people with vascular dementia
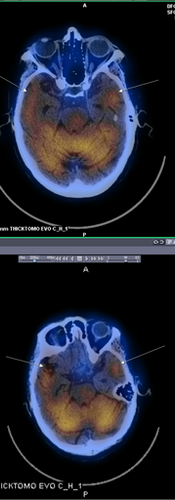
In this single case report, we present a patient diagnosed with vascular dementia by neurocognitive testing and supported by single-photon emission computerized tomography (SPECT) scan imaging with possible frontotemporal lobar degeneration who showed an improvement in symptomatology and cerebral blood flow after 5 months of supportive treatment with photobiomodulation therapy (PBMT) in conjunction with traditional management modalities.
Case Profile:
The patient was a 73 y/o woman who presented with a 6 month history of progressive mood and behavioral disturbances with short-term memory loss. She was brought in by her daughter who described her symptoms as forgetting names, difficulty recognizing familiar faces, getting lost in familiar surroundings, developing inappropriate behaviour and visual and auditory hallucinations. Symptoms were subacute in onset, began approximately 6 months ago and was slowly progressive in nature, prompting the initial visit for assessment and possible treatment.
The patient and her daughter reported no previous history of trauma, cerebrovascular accidents, and neurological or psychiatric disorders. There was a negative family history of cognitive, psychiatric or neurodegenerative disorders. The patient has a medical history of hypertension, ischemic heart disease, dyslipidemia and underwent a previous angioplasty. She is currently on maintenance Simvastatin 20 mg, Bisoprolol 20 mg, Losartan/HCTZ 100 mg/25 mg, Acetylsalicylic Acid 81 mg and Calciferol 5000u.
Physical examination was unremarkable. On neurological examination no aphasia, facial weakness, or hemiparesis were noted. A Mini Mental Status Examination (MMSE) performed revealed a score of 22/30, losing points on orientation to time [2/5], and place [3/5], attention (2/5) and language (7/9). A ‘glove and stocking’ distribution sensory loss was noted. However, nerve conduction studies were normal. Laboratory examinations were unremarkable except for slightly elevated serum creatinine, urea and thyroid stimulating hormone levels. Electroencephalography (EEG) performed revealed normal awake EEG findings.
A cranial MRI performed February 3, 2022 revealed mild degenerative and vascular brain changes consistent with a normal aging brain. A SPECT scan performed the following day revealed patchy reduced perfusion in bilateral frontotemporal lobes and left subcortical structures suggestive of a vascular type dementia. Differentials suggested include frontotemporal lobar degeneration and in light of the reduced volume structurally at the hippocampal formations, Alzheimer type dementia.
The patient was started on oral once a day Risperidone 0.5 mg, Quetiapine 25 mg and Memantine 10 mg. PBMT was applied simultaneously in the clinical outpatient setting as an adjunct to standard medical treatment for vascular dementia. Supervision and monitoring of eating patterns, sleep, and behaviour were done at home with family members.
The following table describes the treatment regimen utilizing the BioFlex Professional System, comprised of the DUO 240+ (240 bicolour Light Emitting Diodes arranged parallel in an array. Biocolour LED diodes exude both 660 nm wavelength and 840 nm wavelengths. Also included in the system are 2 laser diode probes (LDR-100: 660 nm wavelength AlGaInP Laser max power at 100mW; LDI-200: 825 nm wavelength GaAlAs Laser max power at 200mW).
Treatment 1: Administered over Cervical Spine
Treatment 2 and 3: Administered over Cervical Spine and Cranial
Treatment 4, 5 and 6: Administered over Cranial
Treatment 7 and 8: Administered over Cervical Spine
Treatment 9: Administered over Cranial plus Brainstem probe
Treatment 10: Administered over Cervical Spine plus Brainstem probe
Treatment 11 and 12: Administered over Cranial plus Brainstem probe
Treatment 13: Administered over Cervical Spine, Cranial plus Brainstem probe
Treatment Head Wavelength | Frequency (Hz 5 μs resolution) | Duty Cycle (10% steps) | Duration (sec) | Average Power Output (mW) | Power Density (mW/cm2) | Energy (J) | Energy Density (J/cm2) |
DUO +240* |
|
|
|
|
|
|
|
660 nm | CWƗ |
| 300 | 1000 | 10 | 300 | 3 |
840 nm | 10 | 20 | 360 | 400 | 4 | 144 | 1.44 |
Laser Diodes** |
|
|
|
|
|
|
|
LDR-100 660 nm (100% power) | CWƗ |
| 7 | 75 | 750 | 0.525 | 5.25 |
LDI-200 825 nm (20% power) | CWƗ |
| 7 | 36 | 360 | 0.245 | 2.45 |
LDI-200 825 nm (Brainstem Probe*** option) | 1000 | 90 | 7 | 162 | 1620 | 1.134 | 11.34 |
*DUO+240 Arrays (33 minutes total for 3 placements): RED 180 LEDs, wavelength 660 nm. Spot size 100 cm2, IR (Infrared) 180 LEDs, wavelength 840 nm. Spot Size: 100 cm2
**Laser Probes (spot treatment 7 seconds per point spread and distributed across areas covered by arrays, total treatment time 5 min. Spot size 0.10 cm2):
***Brainstem Probe (spot treatment 7 seconds per point spread and distributed across areas covered by arrays, total treatment time 2 min. Spot size 0.10 cm2)
ƗCW – Continuous Wave Mode / Unpulsed
PBMT was provided once to twice a week over 12 weeks utilizing 3 placements in the cervical spine described in image 1 and 3 placements in the cranium described in image 2.

Image 1 Cervical Spine Placements

Image 2 Cranial Placements
3 months after her last PBMT treatment, a repeat SPECT scan was requested. All medications were continued during and after PBMT per standard of care. Repeat SPECT scan revealed an interval moderate improvement in perfusion in the left superior frontal lobe, left side basal ganglia and left side thalamus. The other previously detected areas of hypoperfusion remain stable and no new areas of hypoperfusion were identified. A second MMSE was performed revealing a score of 27/30. She gained points on orientation to time (5/4), attention (5/5) and language (9/9). Image 3
After showing improvement in cerebral blood flow on the left side, maintenance therapy focusing on the right brain was commenced once a week.
Image 3 SPECT analysis
Discussion:
The overall prevalence of dementia in adults older than 50 years in Africa was estimated to be about 2.4%, which translates to 2.76 million people living with a disease in 2010. About 2.10 millions of them live in Sub–Saharan Africa. Prevalence was the highest among females aged 80 and over (19.7%) and there was little variation between regions. Alzheimer disease was the most prevalent cause of dementia (57.1%) followed by vascular dementia (26.9%). The main risk factors were increasing age, female sex and cardiovascular disease.
Patients with cerebrovascular disease who develop dementia or cognitive impairment tend to show various pathologies captured by imaging studies. Conceptually, neuroimaging techniques can be classified into two approaches; structural and functional. Structural imaging refers to approaches that are specialized for the visualization and analysis of anatomical properties of the brain. Structural approaches are particularly useful for detecting brain damage and abnormalities4. In this case, an MRI did reveal structural changes, but these were consistent with a normal aging. Functional brain imaging technologies such as fMRI and PET scans, on the other hand, measure metabolism and/or blood flow and the results are often used in conjunction with structural imaging techniques like MRI or CT.
Brain single-photon-emission-computed-tomography (SPECT) imaging, specifically, has accumulated a wide array of uses relevant to the field of clinical neuropsychiatry, including dementia, traumatic brain injuries, seizures, cerebrovascular disease, complex neuropsychiatric presentations, and treatment-resistant disorders. Perfusion deficits in the frontal lobes and temporal lobes are typical SPECT neuroimaging patterns seen in frontal lobe dementia.
Despite the SPECT findings, this patient displayed symptom patterns more consistent with Alzheimer’s or vascular-type dementia, and medical treatment was directed to address this. Atypical antipsychotics (Risperidone, Quetiapine) and N-Methyl-D-aspartate (NMDA) receptor antagonists (Memantine), useful medications for Alzheimer’s type dementia, in clinical trials have also shown some benefit for vascular-type dementia. The same also applies for the systemic medications this patient is taking to control her hypertension.
PBMT has at the core of its mechanism of action the absorption of certain wavelengths of light, usually red and near infrared, by cytochrome C oxidase (CCO), a terminal enzyme of the electron transport chain that mediates the electron transfer from cytochrome c to molecular oxygen and therefore influences the mitochondrial membrane potential and the consequent processes that follow such as Adenosine Triphosphate (ATP) production and the release of Nitric Oxide (NO). Neural tissues contain large amounts of mitochondrial CCO. Red and NIR photonic energy modulates reactive oxygen species, activates mitochondrial DNA replication, increases early-response genes, increases growth factor expression, induces cell proliferation, and alters nitric oxide levels. Nitric oxide (released locally) has been shown in studies to affect regional cerebral blood flow. This has led to interest on the use of PBMT off-label at least as an adjunctive treatment for certain neurological conditions, from concussions, neurodegenerative disorders, cerebrovascular accidents and dementia.
In this case study, SPECT analysis revealed an improvement in CBF 5 months after treatment with PBMT.
Although studies have shown that antihypertensive medications like Losartan may improve CBF, this was already prescribed to the patient for maintenance. Antipsychotic medications, as well as Memantine has also been shown in some studies to improve cerebral blood flow. Other studies, though, have been able to demonstrate that changes in CBF due to antipsychotic administration may not be the cause of the volumetric changes observed in previous studies, and that other factors should be considered to account for this.
Further, we are intrigued as to why only the left frontal, basal ganglia and thalamic cerebral regions had a moderate improvement in CBF in this patient.
We are proposing the possibility that PBMT may have played a role on this patient’s recovery, as well as on the improvement in cognitive function documented by her MMSE scores.
Further studies on the effects of other adjunctive therapies like physical therapy and occupational therapy might also be helpful.
Our group is also observing whether targeted PBMT on a specific side of the brain as opposed to the systemic effect of remote photobiomodulation will have an effect on regional blood flow on the right side.
References:
1.) https://www.alz.org/alzheimers-dementia/what-is-dementia/types-of-dementia/vascular-dementia. Accessed June 28, 2022
2.) Wolters FJ, et al. Epidemiology of Vascular Dementia. Arterioscler Thromb Vasc Biol. 2019 Aug;39(8):1542-1549. doi: 10.1161/ATVBAHA.119.311908. Epub 2019 Jul 11. PMID: 31294622.
3.) George-Carey R, Adeloye D, Chan KY, Paul A, Kolčić I, Campbell H, Rudan I. An estimate of the prevalence of dementia in Africa: A systematic analysis. J Glob Health. 2012 Dec;2(2):020401. doi: 10.7189/jogh.02.020401. Erratum in: J Glob Health. 2012;2(2):020401corr. PMID: 23289076; PMCID: PMC3529309.
4.) Hirsch GV, Bauer CM, Merabet LB. Using structural and functional brain imaging to uncover how the brain adapts to blindness. Ann Neurosci Psychol. 2015;2:5. Epub 2015 Aug 13. PMID: 30288502; PMCID: PMC6168211.
5.) Medical Advisory Secretariat. Functional brain imaging: an evidence-based analysis. Ont Health Technol Assess Ser. 2006;6(22):1-79. Epub 2006 Dec 1. PMID: 23074493; PMCID: PMC3379170.
6.) Crosson B, et al. Functional imaging and related techniques: an introduction for rehabilitation researchers. J Rehabil Res Dev. 2010;47(2):vii-xxxiv. doi: 10.1682/jrrd.2010.02.0017. PMID: 20593321; PMCID: PMC3225087.
7.) Amen DG, Easton M. A New Way Forward: How Brain SPECT Imaging Can Improve Outcomes and Transform Mental Health Care Into Brain Health Care. Front Psychiatry. 2021 Dec 10;12:715315. doi: 10.3389/fpsyt.2021.715315. PMID: 34955905; PMCID: PMC8702964.
8.) Saura H, et al. Effect of combination therapy with the angiotensin receptor blocker losartan plus hydrochlorothiazide on brain perfusion in patients with both hypertension and cerebral hemodynamic impairment due to symptomatic chronic major cerebral artery steno-occlusive disease: a SPECT study. Cerebrovasc Dis. 2012;33(4):354-61. doi: 10.1159/000335836. Epub 2012 Mar 14. PMID: 22433127.
9.) Griffith DN, et al. The effect of beta-adrenergic receptor blocking drugs on cerebral blood flow. Br J Clin Pharmacol. 1979 May;7(5):491-4. doi: 10.1111/j.1365-2125.1979.tb00991.x. PMID: 38822; PMCID: PMC1429570.
10.) Hamblin M. Mechanisms and Mitochondrial Redox Signaling in Photobiomodulation. Photochem Photobiol, 2018, 94: 199–212.
11.) Chung H, et al. The nuts and bolts of low-level laser (light) therapy. Ann Biomed Eng. 2012;40(2):516–533.
12.) Wu HM, et al. Redefining the pericontusional penumbra following traumatic brain injury: evidence of deteriorating metabolic derangements based on positron emission tomography. J Neurotrauma. 2013;30(5):352–360.
13.) Ilic S, et al. Effects of power densities, continuous and pulse frequencies, and number of sessions of low-level laser therapy on intact rat brain. Photomed Laser Ther 2006; 24(4):458–466.
14.) Hamblin MR. Shining light on the head: Photobiomodulation for brain disorders. BBA Clin. 2016 Oct 1;6:113-124.
15.) Papadopoulos P, et al. Losartan improves cerebrovascular function in a mouse model of Alzheimer's disease with combined overproduction of amyloid-β and transforming growth factor-β1. J Cereb Blood Flow Metab. 2017 Jun;37(6):1959-1970. doi: 10.1177/0271678X16658489. Epub 2016 Jan 1. PMID: 27389178; PMCID: PMC5464692.
16.) Kehoe PG, et al. Safety and efficacy of losartan for the reduction of brain atrophy in clinically diagnosed Alzheimer's disease (the RADAR trial): a double-blind, randomised, placebo-controlled, phase 2 trial. Lancet Neurol. 2021 Nov;20(11):895-906. doi: 10.1016/S1474-4422(21)00263-5. PMID: 34687634; PMCID: PMC8528717.
17.) Araki T, et al. The effects of combine treatment of memantine and donepezil on Alzheimer's disease patients and its relationship with cerebral blood flow in the prefrontal area. Int J Geriatr Psychiatry. 2014 Sep;29(9):881-9. doi: 10.1002/gps.4074. Epub 2014 Jan 17. PMID: 24436135.
18.) Hawkins PCT, et al. An investigation of regional cerebral blood flow and tissue structure changes after acute administration of antipsychotics in healthy male volunteers. Hum Brain Mapp. 2018 Jan;39(1):319-331. doi: 10.1002/hbm.23844. Epub 2017 Oct 23. PMID: 29058358; PMCID: PMC6866296.
19.) Michels L, et al. Baseline Perfusion Alterations Due to Acute Application of Quetiapine and Pramipexole in Healthy Adults. Int J Neuropsychopharmacol. 2016 Dec 3;19(11):pyw067. doi: 10.1093/ijnp/pyw067. PMID: 27466220; PMCID: PMC5137281.
20.) Gordon LC, Johnstone DM. Remote photobiomodulation: an emerging strategy for neuroprotection. Neural Regen Res. 2019 Dec;14(12):2086-2087. doi: 10.4103/1673-5374.262573. PMID: 31397343; PMCID: PMC6788247.









Comments